Clinical Update – Changes to recommended management of borderline RHD in Australia
By Sara Noonan
Borderline RHD
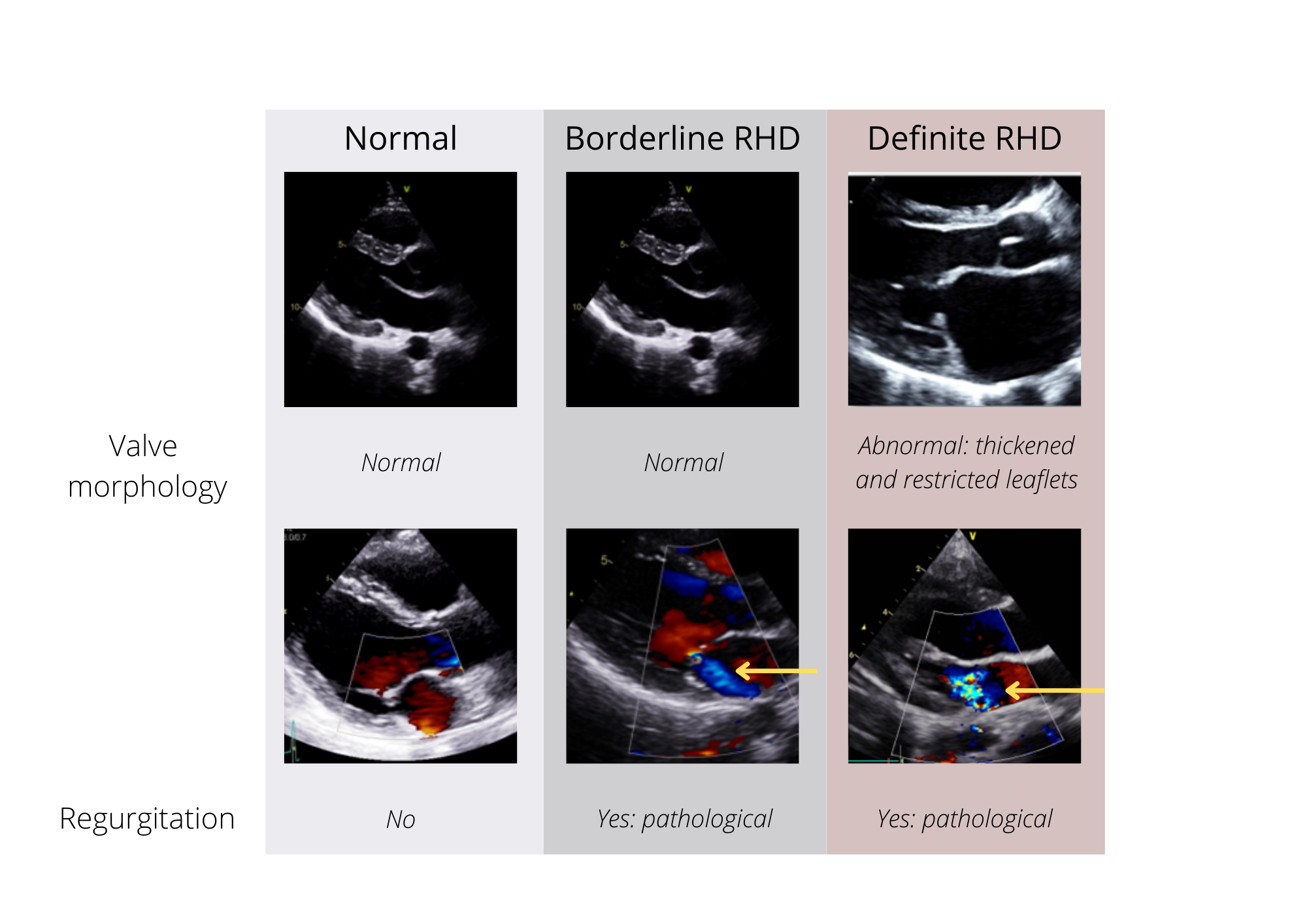
Borderline RHD is defined as echocardiographic features which are abnormal but do not fulfil criteria for the diagnosis of RHD. Borderline RHD is thought to represent both a combination of normal variations in heart echocardiogram findings and early RHD pathology. In people aged over 20 years, minor age-related or degenerative changes may overlap with what is defined as borderline RHD on echocardiography. Therefore, the diagnosis of borderline RHD is restricted to people aged up to and including 20 years of age.
Echocardiography is the primary clinical tool for diagnosis using the World Heart Federation criteria for borderline RHD1 which requires either
- At least two morphological features of RHD of the mitral valve without pathological mitral regurgitation or mitral stenosis, or
- Pathological mitral regurgitation, (without morphological features of RHD of the mitral valve), or
- Pathological aortic regurgitation (without morphological features of RHD of the aortic valve).
Previously in Australia, secondary prophylaxis was not routinely recommended for borderline RHD. It could be considered, however, if there was a personal history of ARF or a family history of rheumatic valve surgery, or if the family preferred treatment.
New evidence
In 2021, researchers working on a large, randomised control trial of secondary antibiotic prophylaxis in Ugandan children and adolescents aged 5 to 17 years with latent mild or borderline asymptomatic RHD published their results; Determining the Impact of Penicillin in Latent RHD: The GOAL Trial.2 They found that children and adolescents with borderline RHD who received secondary prophylaxis for two years after diagnosis were significantly less likely to develop structural heart changes as seen on echocardiography when compared to those that did not receive prophylaxis.
An Australian expert assessment group reviewed these results and after carefully considering the potential benefits as well as possible adverse effects of penicillin and the impact on children and family life, they agreed that the potential benefits of secondary prophylaxis for borderline RHD were clear and applicable to the Australian RHD context.
Updated recommendations
Based on this study the recommendations for managing borderline RHD in Australia have changed. From March 2022, individuals aged 20 years and younger who have no documented history of ARF, are diagnosed with borderline RHD on echocardiogram and who live in a high-risk setting should receive secondary prophylaxis for a minimum of two years following diagnosis. Medical review and repeat echocardiogram should be conducted at 1-2 years after diagnosis, and again 1-2 years after ceasing secondary prophylaxis.3
High risk individuals include
- people living in an ARF-endemic setting,
- Aboriginal and/or Torres Strait Islander peoples living in rural or remote settings,
- Aboriginal and/or Torres Strait Islander peoples, and Māori and/or Pacific Islander peoples living in metropolitan households affected by crowding and/or lower socioeconomic status, and
- people with a personal history of ARF.
Secondary prophylaxis
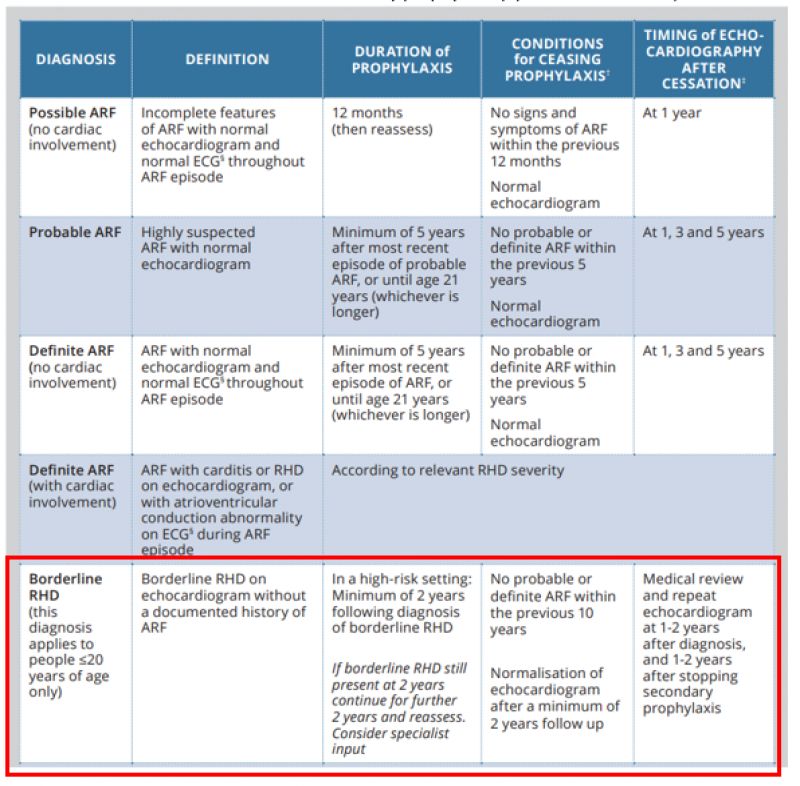
Regular antibiotic prophylaxis helps prevent recurrences of ARF and is crucial in the prevention of RHD. The Australian clinical guideline Table 10.2 (below) has been updated to highlight the recommended duration of secondary prophylaxis with timing of follow up echocardiography.
Table 10.2. Recommended duration of secondary prophylaxis (updated March 2022)
Recommended follow-up
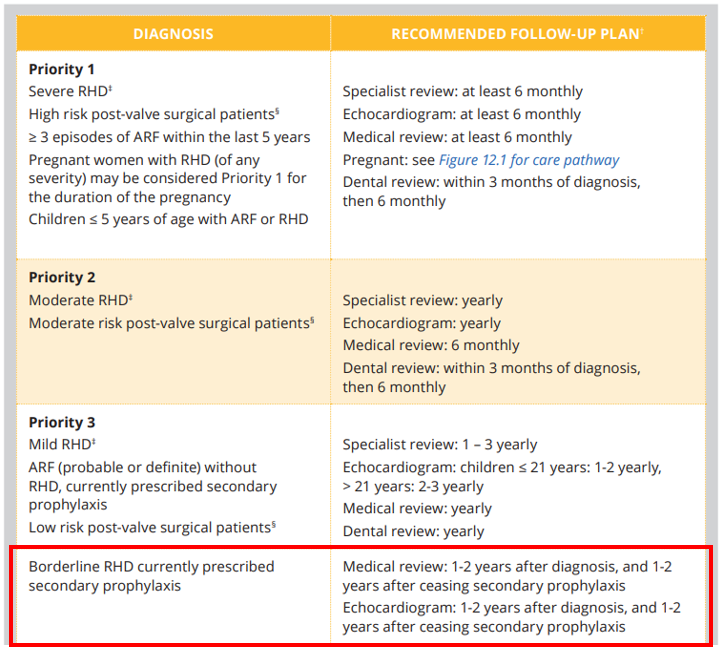
Recommended follow-up planning for RHD has been designed specifically for Australia’s high-risk population based on disease severity. The frequency of each element of care should be tailored to the needs of the individual and may change over time.
Borderline RHD remains a Priority 3 classification, however, management of borderline RHD deviates from the other Priority 3 criteria (below) and is outlined separately.
Table 7.4 / 11.2. RHD priority classification and recommended follow-up (updated March 2022)
The updated management regimen for borderline RHD should start from March 2022, and people diagnosed with borderline RHD before this date should continue with their current care plan.
It is acknowledged that the increased level of care for people diagnosed with borderline RHD, particularly during RHD screening activities, has implications for health staff who administer benzathine benzylpenicillin (Bicillin) injections, and for clinicians planning long-term care involving serial echocardiography.
The WHF 2012 criteria for echocardiographic diagnosis of RHD are currently being updated and are due to be published in 2022. RHDAustralia will announce the publication of this and any subsequent changes to the Australian Guideline after a period of review.
For more information visit the RHDAustralia website.
- 1. Reményi B, Wilson N, Steer A, et al. World Heart Federation criteria for echocardiographic diagnosis of rheumatic heart disease—an evidence-based guideline. Nature Review Cardiology, 2012. 9: 297-309. https://doi.org/10.1038/nrcardio.2012.7
- 2. Beaton A, Okello E, Rwebembera J, et al. Secondary antibiotic prophylaxis for latent rheumatic heart disease. N Engl J Med 2022; 386:230-240 https://doi.org/10.1056/NEJMoa2102074
- 3. RHDAustralia (ARF/RHD writing group). The 2020 Australian guideline for prevention, diagnosis and management of acute rheumatic fever and rheumatic heart disease (3.2 edition, March 2022); 2020
